
Last reviewed: 30 June 2025
Last reviewed: 30 June 2025
99.8% of all cervical cancer cases in the UK are caused by HPV infection
. Most sexually active people come into contact with HPV during their lifetime. Usually the virus causes no harm and the infection clears on its own. However, in some cases, HPV infection can lead to cell changes that can progress into cervical cancer.HPV primary screening is now embedded in primary care across the UK as it identifies people at a higher risk of developing cervical cancer and it’s a more accurate test than the previous approach of cytology. This means that cervical cell samples are tested for HPV and only samples that are HPV positive will be examined in the lab for any changes in the cells. People who are HPV positive and cytology negative are invited for yearly surveillance.
It has been estimated that HPV primary screening in England may reduce the number of cervical cancers in women aged 25–64 by 23.9%, saving even more lives and helping to avoid unnecessary procedures for women
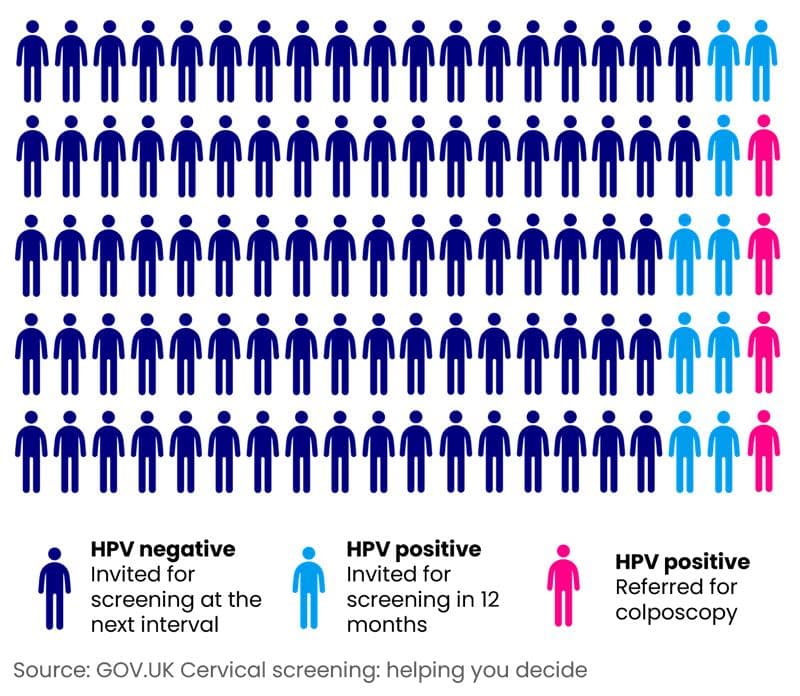
.The diagram below shows that for every 100 people screened, 87 would be HPV negative. Following cytology of the HPV positive samples, only 4 people would have abnormal cell changes identified and would be referred for colposcopy.
Read more about HPV and the HPV vaccination.
The HPV vaccination reduces the chance of someone being infected with HPV. The Gardasil 9 vaccine is currently supplied for those eligible for the HPV vaccine and protects against 9 strains of the virus
. The HPV vaccine is expected to prevent up to 90% of cervical cancers. There is great potential for HPV vaccination to lead to the elimination of cervical cancer as a public health problem. In addition, HPV is linked to non-cervical cancers such as head and neck cancer and therefore has wider positive impacts for cancer control.People who’ve been vaccinated against HPV should still participate in cervical screening as there is still a small chance that vaccinated people can get cervical cancer
. Primary care have a role to play in raising awareness of the fact that cervical screening is still important as the vaccine does not protect against all strains of the virus and doesn’t provide 100% immunity.All children aged 12 to 13 are offered the HPV vaccination in schools. The programme started in 2008 for girls, and in 2019 it was expanded to boys to further prevent the potential spread of the virus, as well as to protect against male HPV related cancers.
In 2018, a HPV vaccination programme for men who have sex with men was implemented to ensure this group are offered protection against male HPV related cancers too.
These recent changes mean that there are people eligible for the vaccine who may not have received it. In your practice, make sure you check the HPV vaccination record and offer the vaccine to all girls under 25 and boys born from September 2006 up until their 25th birthday. Men who have sex with men under 45 can access HPV vaccination through sexual health clinics.
If an eligible child misses getting their HPV vaccine at school, they can be vaccinated at a catch-up clinic. If you are unsure when or where these clinics are in your area contact your local immunisation team or health board.
For more information about changes to HPV vaccination, including doses for different groups, go to the GOV.UK HPV vaccination guidance
There has been a decline over the past 10 years in the number of people taking up their offer of cervical screening.
Cervical screening coverage is the percentage of eligible people invited for screening who have had a test with a recorded result within a specified period. Coverage across the UK ranges from 66.7% to 69.9% (data from 2021/22)
.Lower attendance is particularly evident in the youngest as well as the oldest age groups
, and in underserved groups such as those from lower socio-economic and ethnic minority backgrounds.Our primary care good practice guide (PDF, 1.57 MB)details how you can encourage informed participation and reduce access barriers to ensure the cervical screening programme is effective.
Find statistics for your nation:
In England, Wales and Northern Ireland, cervical screening uptake is incentivised through the Quality and Outcomes Framework (QOF), where practices need to ensure a high proportion of the target cohort undergo screening regularly to receive payment.
In England, the QOF Quality Improvement module on the early diagnosis of cancer(PDF) provides an opportunity for GP practices to develop quality improvement plans for all screening programmes.
In England, the Primary Care Network (PCN) GP Contract Requirements for the Early Diagnosis service specification asks PCNs to contribute to improving local uptake of screening by working with local system partners. For more information read our GP contract hub.
There are currently no national incentive schemes operating in Scotland, but this may change in the future. In Scotland, each health board has a Screening Inequalities plan covering quality improvement activity. Training for NHS staff is available on TURAS. The Scottish Equity in Screening Strategy 2023-2026 provides an overview of current national projects to support the reduction of screening inequalities, which may be of interest to health professionals in Scotland.
Even without incentive schemes in place, it’s important to remember the valuable role that primary care can play in helping to support informed uptake of screening, removing any barriers and working collaboratively with local partners to reach out to communities.

The latest evidence on barriers and actions to support people to access cervical screening.

Covers extending screening intervals, self-sampling and wider quality improvements.

Get resources to support uptake, including information on safety netting and barriers to participation.
Brown, K.F. et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer, 2018.
Castanon A, Landy R, Sasieni P. By how much could screening by primary human papillomavirus testing reduce cervical cancer incidence in England?. J Med Screen. 2017.
Falcaro M et al, The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study, Lancet, 2021
NHS digital. Cervical Screening Programme, England - 2022-2023.
Douglas, E., et al. Socioeconomic inequalities in breast and cervical screening coverage in England: are we closing the gap? Journal of Medical Screening. 2015
Urwin, S. et al., Factors associated with cervical screening coverage: a longitudinal analysis of English general practices from 2013 to 2022, Journal of Public Health. 2023.
Stay up-to-date with the latest cancer research information.