Surgery for vulval cancer
There is a risk of problems or complications after any operation. The possible complications may include bleeding, urinary tract infections and wound infections. Infections of the wound may cause wound breakdown, delayed wound healing and poor cosmetic result after surgery
Many problems are minor but some are more serious. Treating them as soon as possible is important.
You are very unlikely to get all the side effects or problems we cover here. Which side effects you have, depends on the type of operation you have had. Generally speaking, the smaller the operation, the fewer the side effects.
Read about the types of surgery for vulval cancer
It can take time to come to terms with surgery and the possible side effects. Many women feel different emotions. How you feel can change daily, this is a natural part of coming to terms with your cancer treatment. It is difficult to say how you will feel and how quickly you will recover, everyone is different.
Some women may choose to look at the vulval area soon after surgery, while others prefer to wait. There is no right or wrong way. It is important that you feel ready. Your nurse can be with you the first time you do this.
As you have had surgery on a very intimate part of your body, you may feel less attractive or sexual. You may feel embarrassed about how your genital area looks now.
Talk to your GP, doctor or specialist nurse if you are struggling. They can suggest different things to help you such as counselling. Talking to someone who isn't closely involved can be very helpful and give you the listening time you need.
Read more about coping with vulval cancer and who can help
You are at risk of getting an infection after an operation. This includes a wound, chest or urine infection. Symptoms can depend on where the infection is. Tell your doctor or nurse if you have any symptoms of infection.
These include:
a high temperature
shivering
feeling hot and cold
feeling generally unwell
cough
feeling sick
swelling or redness around your wound and your wound might feel hot
a strong smell or liquid oozing from your wound
loss of appetite
cloudy smelly pee
If you get an infection, your doctor gives you antibiotics to treat it.
Sometimes for an infection in your wound, you may need another operation. But this is rare.
Blood clots are also called a deep vein thrombosis or DVT. They are a possible complication of having surgery because you might not move about as much as usual. Clots can block the normal flow of blood through the veins. Let your doctor or nurse know if you have an area in your leg that is swollen, hot, red or sore.
There is a risk that a blood clot can become loose and travel through the bloodstream to the lungs. This causes a blockage called a pulmonary embolism. Symptoms include:
shortness of breath
chest pain
coughing up blood
feeling dizzy or lightheaded
To prevent clots it's important to do the leg exercises that your nurse or taught you. And to move around as much as possible. Your nurse might also give you an injection just under the skin to help lower the risk whilst you are in hospital. You might need to carry on having these injections for a few weeks, even after you go home. This depends on the type of operation you had.
Your nurse might teach you to do these injections yourself before you go home. They will make sure you are comfortable doing them. Or a district nurse might come to your home to do them.
It's important to continue wearing your anti embolism stockings if you have been told to by your doctor.
It is common to have some swelling around the genital area for a couple of weeks after surgery. If this continues or you notice some swelling in your legs or feet, you may be developing lymphoedema.
Lymphoedema is a build up of that causes swelling in a part of the body.
You are more at risk of developing lymphoedema if the surgeon removes lymph nodes in your groin during surgery. This is a lymph node dissection or lymphadenectomy. It may affect one or both legs depending on the type of surgery you had.
Lymphoedema is easier to control if treated early. It is important that you are referred to a lymphoedema specialist if you have signs of swelling. This is usually a nurse or physiotherapist.
There are different treatments for lymphoedema. These include:
specially fitted stockings
manual lymphatic drainage (MLD)
compression bandaging
inflatable sleeves to gently squeeze fluid up towards the top of your legs
It is a good idea to:
Try to protect your legs and feet from sharp objects - don't walk around in bare feet and wear long trousers for gardening.
Wear insect repellent so that you won't get bitten.
Take care of all cuts, scratches or bites without delay, by cleaning with antiseptic and covering with a dressing.
Avoid sunburn.
Take extra care when cutting your toenails - you should not cut or tear the cuticles.
Use an electric razor carefully if you must shave your legs.
Read more about lymphoedema and its treatment
Scar tissue can form around the vulval area after surgery. Scar tissue is stiffer and less stretchy. If scar tissue forms around the outside of your vagina, it may narrow the entrance. You may find penetrative sex painful. Scar tissue may change the shape and size of your remaining vulval tissue.
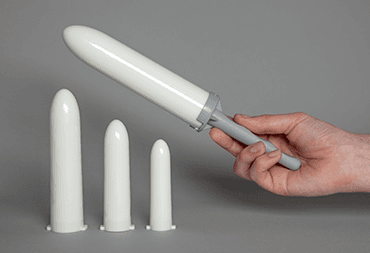
Stretching your vaginal opening with vaginal dilators can help. These are inserted into the vagina for a few minutes each time you use them.
Dilators are smooth cone shaped objects that you put into your vagina to stretch it. They come in different sizes and you can use them with a water soluble lubricating gel.
You begin with one of a comfortable size and use larger ones until your vagina is stretched enough for you to have sex comfortably. This may not be something you feel you can cope with straight after your surgery. Some people like to involve their partner with this, but this is entirely up to you.
Contact your specialist nurse or doctor if you have any problems or questions. A surgeon can sometimes use to widen the vaginal opening if dilators have not worked.
Many women are able to return to having sex after the wound has healed. This can take about 6 to 8 weeks. But for some, it can take months or longer before they are ready for sex after surgery.
It may help to talk to your doctor or nurse who can support you and your partner if you have one. They may refer you to a counsellor who specialises in sexual problems.
After surgery for vulval cancer, you might find sex less pleasurable or have problems reaching orgasm. This is most likely to happen if you've had the clitoris removed. Some women still find sex pleasurable after surgery but it may take some time.
You may also notice numbness in your genital area after a radical vulvectomy. This is due to nerve damage, which can happen during surgery. Nerves do heal, but very slowly. So the feeling may only start to come back months after your surgery.
You can still enjoy a good sex life, but it may just take more time for you to relax and enjoy intimate touch and sex again.
Find out more about sexual relationships after treatment for vulval cancer
Depending on the type of surgery you have had, you may have some nerve damage. This can cause different side effects such as:
tingling
pins and needles
unexplained hot or cold areas
feelings similar to mild electric shocks
complete numbness in some areas of the skin
Where you get these feelings depends on which nerves were damaged. You may have these feelings between your legs, in your groin or down on your legs.
It is important to remember that nerves heal with time. But it may take months or even years for them to fully heal. Slowly, the problems should lessen.
Rarely, some women may have permanent nerve damage. This means that these side effects won't go away completely, but they should still improve over time.
Most women who have surgery for vulval cancer will not have any problems with their bladder or bowel.
In the first few weeks after surgery, it is important to eat well and drink plenty of fluids to avoid constipation. This can delay wound healing if you have to strain when having a poo.
Drinking plenty of fluids also helps reduce the risk of developing an infection in your wee (urinary infection). Your specialist nurse or doctor can give you specific advice about this.
Vulval cancer can sometimes spread from the vulva to other parts of the body such as the bowel, bladder or womb. In these situations, your surgeon may suggest a very large operation that involves bowel or bladder surgery. This is a pelvic exenteration.
This operation is rare for vulval cancer. Your surgeon will only consider this if you are fit enough to make a good recovery.
Read more about pelvic exenteration in the cervical cancer section
Surgery for vulval cancer can be very difficult to cope with. It is important for you to have access to emotional support and information.
Find out about coping with life after treatment for vulval cancer
Last reviewed: 04 Sept 2025
Next review due: 04 Sept 2028
Surgery is the main treatment for vulval cancer. The type of surgery you need depends on how big the cancer is and how much of your vulva is affected.
Coping with vulval cancer can be difficult. There is help and support available to help you.
Your vulval area will be more sensitive after treatments such as surgery or radiotherapy. Find out how you can take area of your vulva after treatment.
Your treatment depends on a number of factors. Surgery is the most common treatment for vulval cancer.
After treatment for vulval cancer, you might have follow up appointments every 3 months. This is usually at the hospital with your doctor or specialist nurse (CNS).
Vulval cancer is a rare cancer. It can start in any part of the female external sex organs, the vulva. The treatment you need depends on how big the cancer is and whether it has spread.
About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.