Radiotherapy for bone cancer
Radiotherapy means the use of radiation, usually x-rays to treat cancer. For bone cancer, doctors use a type of radiotherapy called external radiotherapy.
You don't routinely have radiotherapy for all types of bone cancer. But it can be an important part of treatment for some bone cancers such as Ewing sarcoma.
This page is about cancer that starts in your bone (primary bone cancer). If your cancer has spread into bone from another part of the body, it is called secondary or metastatic bone cancer.
How does radiotherapy work?
Radiotherapy treatment works by damaging the  within the cancer cells. DNA is the genetic code that controls how the body's cells behave.
within the cancer cells. DNA is the genetic code that controls how the body's cells behave.
When do you have radiotherapy for bone cancer?
You don't routinely have radiotherapy for all types of bone cancer. But it can be an important part of treatment for Ewing sarcoma.
For Ewing sarcoma you might have radiotherapy as your main treatment. Or you might have it before or after surgery.
It is less common to have radiotherapy for other types of bone cancer. But you might have it:
- if surgery isn’t possible
- after surgery to help lower the risk of the cancer coming back
- before surgery to shrink the cancer to help make it easier to remove
- to help control the cancer and relieve symptoms
Types of radiotherapy for bone cancer
You have external radiotherapy for bone cancer. External radiotherapy uses a machine from outside of the body. It directs radiation beams at the cancer to destroy it.
This is different to internal radiotherapy which means giving radiotherapy to the cancer from inside the body.
The type of external radiotherapy you have depends on the:
- type of cancer you have
- where it is
- how far it has grown or spread (the stage)
- the treatment you have already had
- your general health
Conformal radiotherapy
Conformal radiotherapy shapes the radiation beams to closely fit the area of cancer. It is also called 3D conformal radiotherapy or 3DCRT. It is a very common type of radiotherapy.
Intensity modulated radiotherapy (IMRT)
IMRT shapes the radiotherapy beam to fit the shape of the tumour very accurately. It delivers different amounts of radiation to different parts of the treatment area. This allows higher doses of radiation to treat the area. The surrounding healthy tissues get less radiation.
Stereotactic body radiotherapy (SBRT)
SBRT gives radiotherapy from many different angles around the body. The beams meet at the tumour. This means the tumour receives a high dose of radiation and the tissues around it receive a much lower dose. This lowers the risk of side effects.
This type of radiotherapy is mainly used to treat very small cancers such as bone cancer that has spread to the lung.
Proton beam therapy
Proton bean therapy radiotherapy uses high energy or low energy proton beams to treat cancer. For bone cancer you have high energy proton beams. This type of radiotherapy uses protons which are small parts of atoms, instead of using high energy x-rays (photons).
You might have this type of radiotherapy for Ewing sarcoma, chordoma and chondrosarcomas.
How long is a course of radiotherapy?
You have radiotherapy as a series of daily treatment sessions. A single dose of radiotherapy is called a fraction. A series of sessions makes up a radiotherapy course. You usually have a fraction every day, from Monday to Friday, with a rest at the weekend.
The number of fractions you need depends on your individual situation. A course of radiotherapy may be 1 week or it can be as long as 8 weeks. Your doctor will explain how long you will have radiotherapy for.
Radiotherapy to relieve cancer symptoms such as pain is called palliative radiotherapy. You often have this in fewer fractions. Sometimes it is just one treatment. Palliative radiotherapy has fewer side effects. Your doctor will discuss with you how many sessions you need.
Planning radiotherapy for bone cancer
Before you begin your treatment, the radiotherapy team carefully plan your external beam radiotherapy. This means working out how much radiation you need to treat the cancer and exactly where you need it.
Your planning appointment may take from 15 minutes to 2 hours. You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
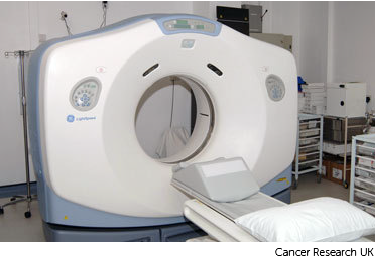
Your radiographers tell you what is going to happen. They help you into position on the scan couch.
The CT scanner couch is the same type of bed that you lie on for your treatment sessions. You need to lie very still. Tell your radiographers if you aren't comfortable.
Injection of dye
You might need an injection of dye (contrast) into a vein. This is through a small tube that goes into the back of your hand. It’s called a cannula. The contrast helps body tissues show up more clearly on the scan.
Before you have the contrast, your radiographer asks you about any medical conditions or allergies. Some people are allergic to the contrast.
Having the scan
Once you are in position your radiographers put some markers on your skin. They move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 5 minutes. You won't feel anything. Your radiographers can see and hear you from the CT control area where they operate the scanner.
Ink and tattoo marks
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.

The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
Radiotherapy masks and moulds
Your treatment team might make a plastic mould or mask for you. This is also called a shell. This is to keep your arm or leg still during the treatment sessions. This is so your treatment will be as accurate as possible.
Most types are made of a mesh material with lots of small holes. You can have a mould for other parts of the body, such as the chest, head or neck.
You wear the mould or mask for each treatment session. The radiographers might make marks on it. They use the marks to line up the radiotherapy machine for each treatment.
Vacuum bag mould
A vacuum bag mould is used during your treatment to help keep you still and in the right position.
Your radiographer might make a mould using a plastic cushion filled with tiny polystyrene balls.
They mould the cushion around the treatment area and then suck out the air with a vacuum pump.
This moulds the cushion very closely around your body and the radiographer removes the pump. The cushion then forms a solid and firm support each time you have treatment. The cushion is called a vac pac.
After your planning session
You might have to wait a few days or weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This lowers the side effects you might get during and after treatment.
Having radiotherapy
Radiotherapy machines are very big and could make you feel nervous when you see them for the first time. The machine might be fixed in one position. Or it might rotate around your body to give treatment from different directions. The machine doesn't touch you at any point.
Before your first treatment, your  will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.
will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.

Before each treatment session
The radiographers help you to get onto the treatment couch. You will be in the same position that you were in for the planning appointment. If they used a plastic shell at the planning appointment then they will use this again.
The radiographers line up the radiotherapy machine using the marks on your body. Once you are in the right position, they leave the room.
During the treatment
You need to lie very still. Your radiographers might take images (x-rays or scans) before your treatment to make sure that you're in the right position. The machine makes whirring and beeping sounds. You won’t feel anything when you have the treatment.
Your radiographers can see and hear you on a CCTV screen in the next room. They can talk to you over an intercom and might ask you to hold your breath or take shallow breaths at times. You can also talk to them through the intercom or raise your hand if you need to stop or if you're uncomfortable.
You won't be radioactive
This treatment doesn't make you radioactive. You can have visitors while you are in hospital.
Travelling to radiotherapy appointments
You might have to travel a long way each day for your radiotherapy. This depends on where your nearest cancer centre is. This can make you very tired, especially if you have side effects from the treatment.
You can ask your radiographers for an appointment time to suit you. They will do their best, but some departments might be very busy. Some radiotherapy departments are open from 7 am till 9 pm.
Car parking can be difficult at hospitals. Ask the radiotherapy staff if you are able to get free parking or discounted parking. They may be able to give you tips on free places to park nearby.
Hospital transport may be available if you have no other way to get to the hospital. But it might not always be at convenient times. It is usually for people who struggle to use public transport or have any other illnesses or disabilities. You might need to arrange hospital transport yourself.
Some people are able to claim back a refund for healthcare travel costs. This is based on the type of appointment and whether you claim certain benefits. Ask the radiotherapy staff for more information about this and hospital transport.
Some hospitals have their own drivers and local charities might offer hospital transport. So do ask if any help is available in your area.
Side effects of radiotherapy
Radiotherapy for bone cancer can cause side effects, but knowing what to expect can help you to cope with them.
The side effects you get will depend on:
-
where you are having treatment to
-
how much radiotherapy you have (the number or fractions and overall dose)
-
if you have it with other treatments such as chemotherapy
Some of the side effects can include:
-
reddening or darkening of your skin in the treatment area
-
loss of any body hair in the treatment area
-
tiredness and weakness
-
feeling or being sick
-
diarrhoea
The following video talks about the general side effects of radiotherapy. This video is around 8 minutes.
Radiotherapy can cause many different side effects, such as tiredness. The side effects you get will depend on the area you're having treatment to, but there are some general side effects you might experience regardless of where your cancer is. This video is about the general side effects you might have.
On screen text: Tiredness and weakness
Martin (Radiographer): As the normal cells repair themselves from the treatment this can use a lot of the body's resources, causing tiredness.
David: After about four weeks, I started to get tired. The body was starting to weaken.
Laurel: I was tired, day and night. Getting up in the morning was like a chore. I couldn't talk for 5 minutes. I would just sleep and just sleep and just wake up and sleep again.
Martin (Radiographer): Listen to your body. Take rests if you need to. Try not to overdo things.
Laurel: Don't fight with yourself too much. Just like go at a pace and just work with your body. If you can't make it today, you can't make it today.
David: You've got to rest. You have to take the time to rest.
Mary: Just going for them small walks. They really do help you. And even if it is just walking around your house or just walking around the block.
Martin (Radiographer): Doing exercise can help with tiredness by helping you maintain energy levels.
Mary: Being outside, that's a big, massive thing as well because you're feeling the fatigue and I think getting outside, just getting a bit of fresh air that really, really did help me.
Martin (Radiographer): The tiredness you can expect to begin within the first few weeks of treatment. Once it reaches its peak, about two weeks after treatment it recovers quite quickly after that.
Mary: It's not forever. You're not going to be like this forever and I did have to tell myself that.
Laurel: Two months after treatment, I start to feel less tired and that was a way forward because things start to really improve.
On screen text:
Rest and have short naps when you need to
Drink plenty of water
Eat a balanced diet
Do some gentle exercise
Get some fresh air
On screen text: Sore skin
Martin (Radiographer): The radiotherapy can cause soreness of the skin. This only affects the area that you are having treated. This usually starts to appear about two weeks after you start treatment. You may notice this becoming more red and may become more itchy and sore as treatment continues.
David: After about ten days I started to get red on the area that they were targeting and it just progressively got redder and redder.
Laurel: My skin was dry and at the back was just like this triangle shape thing where it was like, okay, I'm a woman of colour, but it was really, really black.
David: Wasn't too painful, it was sort of annoying, rather than painful.
Martin (Radiographer): After treatment’s finished, the skin will remain sore for up to two weeks, but then recovers quite quickly.
Laurel: I haven’t got no scarring now at all.
David: It was maybe three or four weeks and then all the blemishes disappeared front and back.
Martin (Radiographer): When you start treatment we would advise you to carry on with your normal skincare routine but as the side effects develop, then your team will advise you on which products you can use on the skin safely.
Laurel: When I'm washing myself I use a sponge and you're just literally as it were just squirt it down, you don't rub the skin at all because it's already damaged. Pat dry, don't rub.
David: I spoke to the hospital about it and it was them that recommended this cream to put on, just to alleviate the symptoms.
Martin (Radiographer): We'd recommend wearing loose clothing and keeping the treatment area covered up against the sun and wind.
Laurel: I had to change most of my wardrobe. I only wore cotton.
David: Wearing T-shirts, soft clothing, nothing that would rub.
Mary: It's important when you go outside to make sure that you do wear that headscarf, or you do wear a hat or whatever it is.
Laurel: I wouldn't go in the sun at all, at all because my skin was - I know it was too delicate.
On screen text:
Don’t rub the area, press if it is itchy and dab your skin dry
Don’t use perfume, perfumed soaps or lotions on the area
Don’t shave the area
Only use creams or dressings advised by your specialist or radiographer
Wear loose fitting clothing
Avoid strong sun or cold winds
Make sure you wear sunscreen
On screen text: Hair loss
Martin (Radiographer): Radiotherapy can cause hair loss in the area that's being treated, whereas chemotherapy can cause hair loss all over the body.
Mary: 2 to 3 weeks after the radiotherapy, I was brushing my hair and loads came out on the brush. I knew it was going to happen, but it was just hard when it happened.
Martin (Radiographer): In most cases the hair will grow back. This can take a couple of months and the hair may have a slightly different colour or texture.
Mary: Mine did grow back and there's a lot of grey in it so I have to dye it. This is not my original colour. It's very slow growing back.
Martin (Radiographer): Use a simple soap to clean the area. Be gentle with the skin in that area and after washing pat the area dry with a soft towel.
On screen text:
Radiotherapy can make hair fall out in the treatment area
It won’t cause hair to fall out in other parts of your body
Your hair might grow back a few weeks after treatment ends
If your hair won’t grow back, then your doctor should tell you
Don’t use perfume, perfumed soaps, or lotions on the area
On screen text: Your mental health
Laurel: I felt frustrated. Some days were really, really challenging where there were just tears without words.
Mary: It's a mixture of emotions. You feel angry and you feel frustrated. You lose your confidence.
Martin (Radiographer): Radiotherapy can cause a lot of emotions at various times during the treatment. You may feel sad or anxious or depressed, which is quite normal. It's good to talk to people about your experiences, whether that's your team at the hospital or friends and family.
David: I couldn't praise the team highly enough. Everybody that was involved were unbelievable and if it hadn't been for them, I just don't think I would have gotten through with it.
Mary: I did have a nurse as well and she had the experience of dealing with people that went through brain surgery, went through radiotherapy so it was just great that I could reach out.
Martin (Radiographer): Your team will be able to give you information about local patient support services that are available, that includes things like counselling and complementary therapies.
Laurel: A referral from the hospital counselling, which I attended for about a year.
Martin (Radiographer): There's also lots of support available online and in your local area.
Mary: I went on loads of different forums and I spoke to loads of different people and it really, really helped me. If I didn't do that, I don't think I would have got through most days.
Laurel: If you get a bit cranky or feel a bit low, go for it. But there's so much help out there and that's why I'm pushing forward like don't sit down in silence. It's the same thing, just get the help you need.
On screen text:
There is help available – ask the hospital for support
Talk to your friends and family about how you are feeling
Ask about local support groups
Your GP or hospital can provide counselling
You can get help and support online through forums
If you're experiencing a side effect that hasn't been covered in this video, you can find more information on the Cancer Research UK website.
On screen text: For more information go to: cruk.org/radiotherapy/side-effects



